Overview
This Annual Health Report (AHR) is for fiscal year (FY) 2079/80. It serves as a comprehensive document within the health sector, fulfilling the dual purpose of monitoring progress of annual programs and providing a detailed documentation of various facets including the health scenario, guiding documents/milestones, major activities of the fiscal year (FY), program/service status and strategic analysis of the strength, weakness, opportunity, and threat for the programs and service delivery.
The annually compiled comprehensive health sector report stands as a pivotal document, serving as a thorough monitoring and evaluation tool for the progress of planned programs, analysing shifts in coverage and utilization statistics. This indispensable record not only offers a snapshot of the sector’s advancements but also traces its evolution over time. This marks the 29th consecutive publication of its kind and the 7th Annual Report since the reorganization of MoHP.
Rationale
The report serves a dual purpose, functioning as both an annual program monitoring report and a comprehensive document covering various aspects, including:
- Health Scenario: An overview of the prevailing health issues at the federal and provincial level.
- The local level details are included in the respective provincial level annual reports, needful information at programmatic level for local levels have also been included as per need felt by the respective programs
- Guiding documents and milestones: Salient features of the key guiding documents and milestones relevant to health programs.
- Major activities in FY 2079/80: A comprehensive account of the significant activities carried out in health sector and related programs/services during the fiscal year
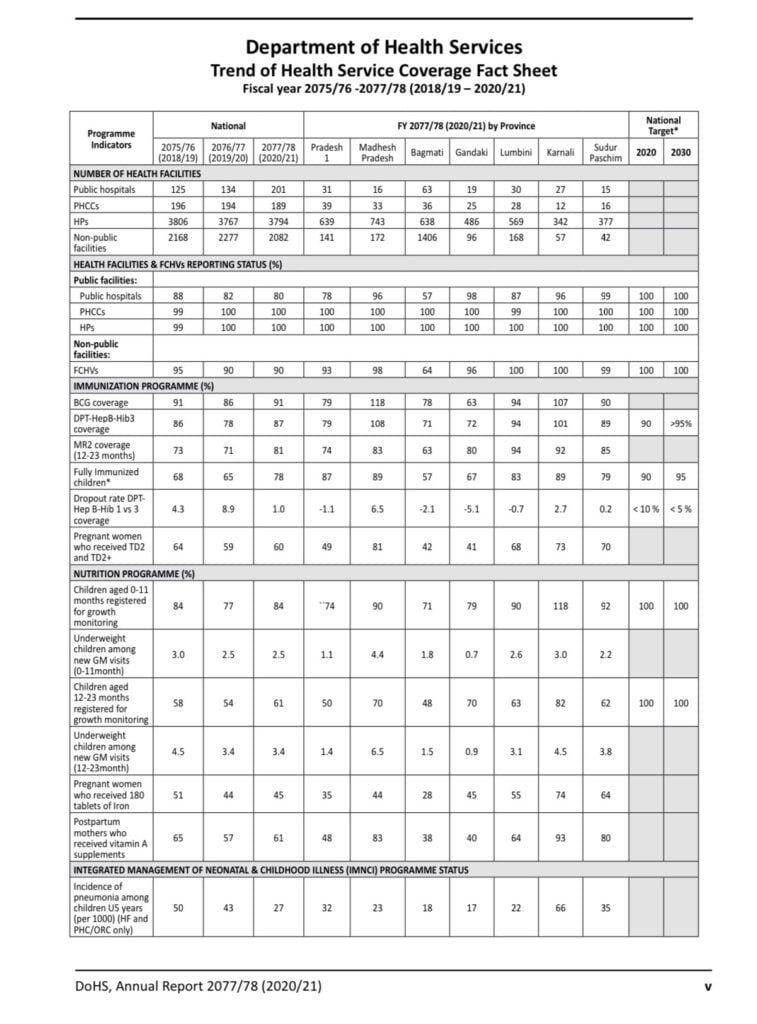
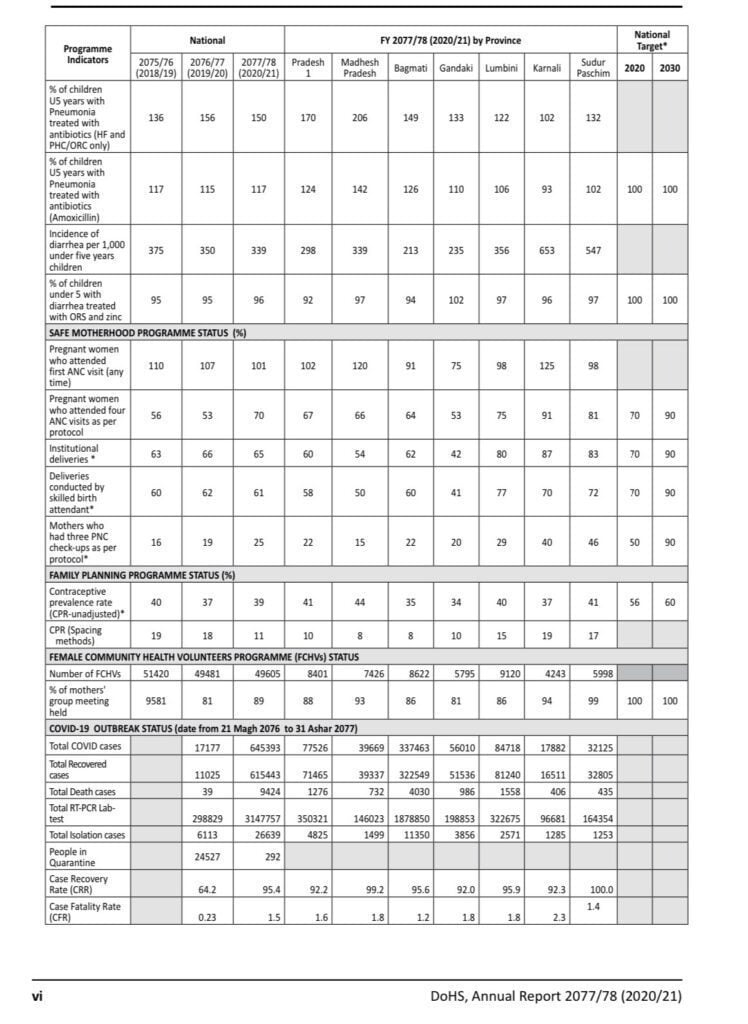
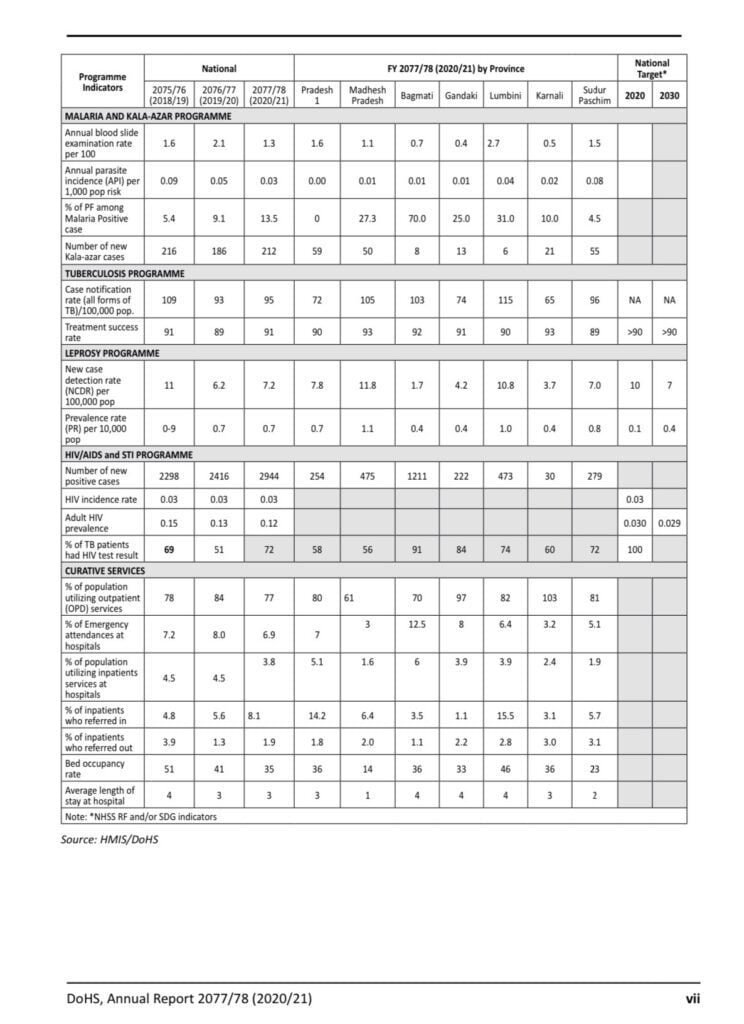
- Status of program/service indicators: Monitoring of the status of the pertinent program/services providing insights into achievements and areas that require attention
- SWOT Analysis: A strategic analysis covering the strength, weakness, opportunity, and threat (SWOT) pertaining to the programs and services.
- The timely release of the annual report assumes crucial importance, as it establishes a vital link between service delivery and evidence-informed decision-making and planning for future programs. This dynamic and insightful report not only reflects the health sector’s current standing but also guides future initiatives towards more effective and impactful healthcare strategies and action.
Related documents
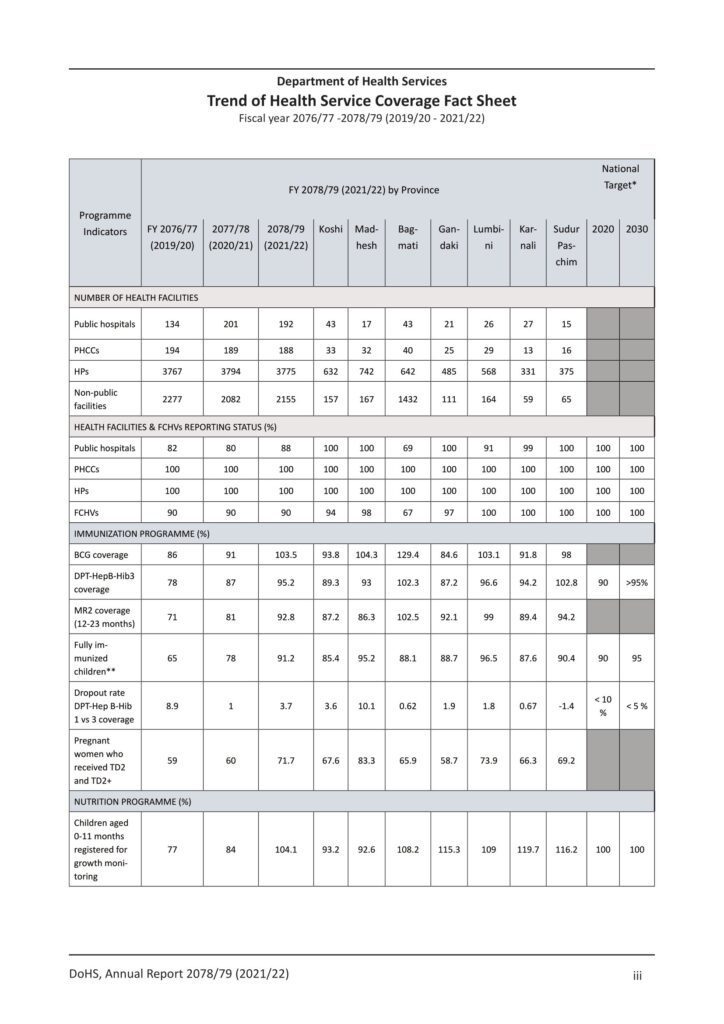
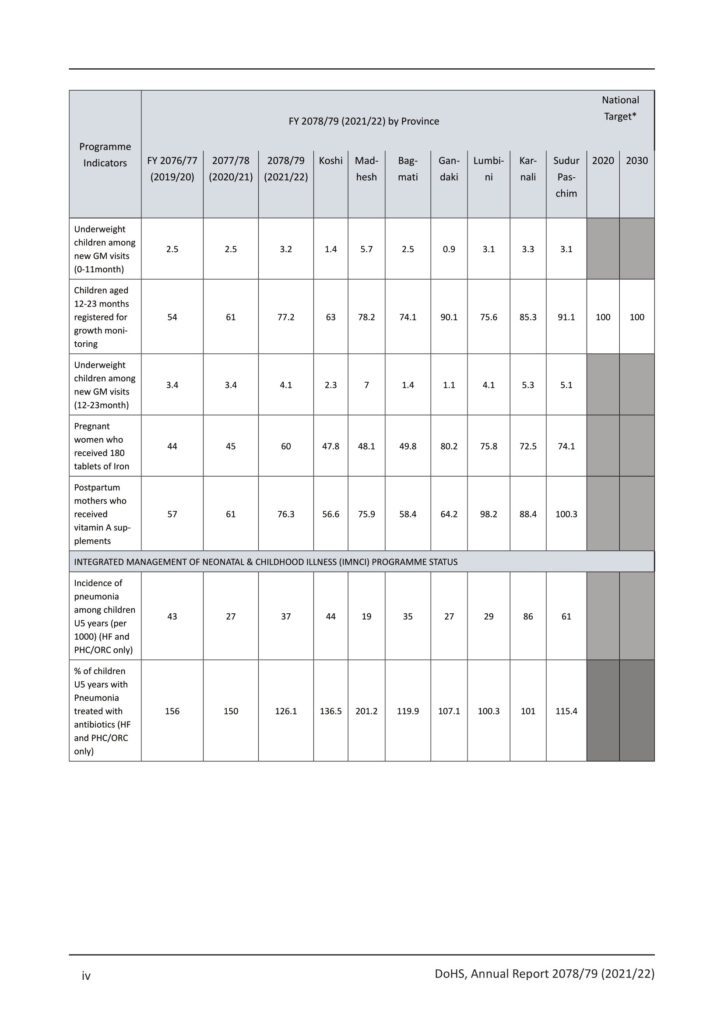
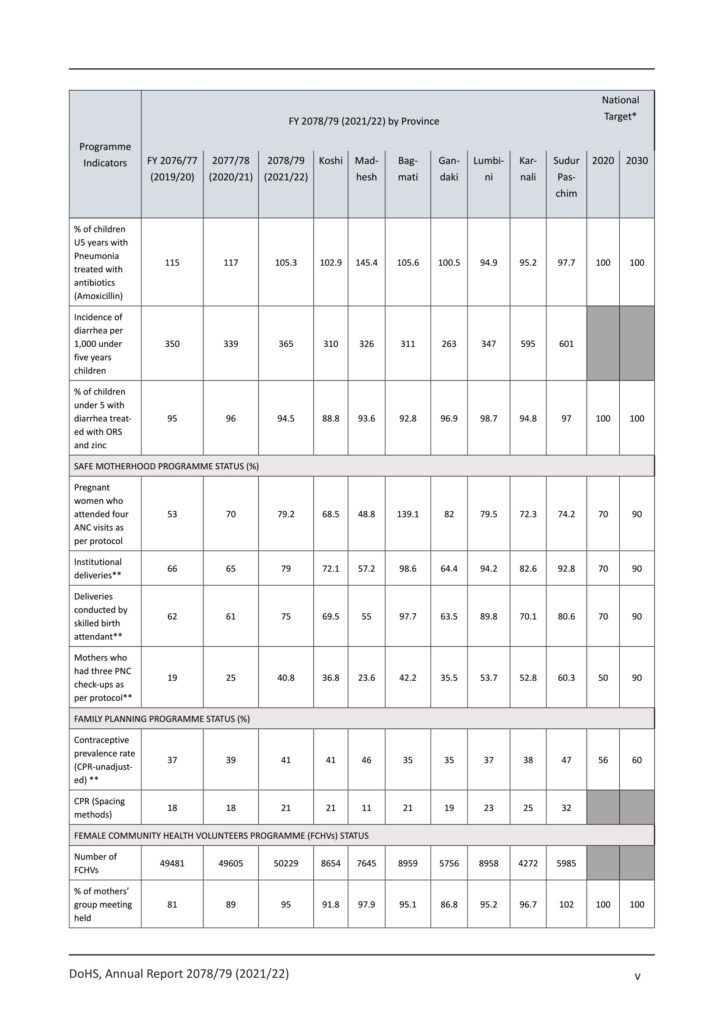
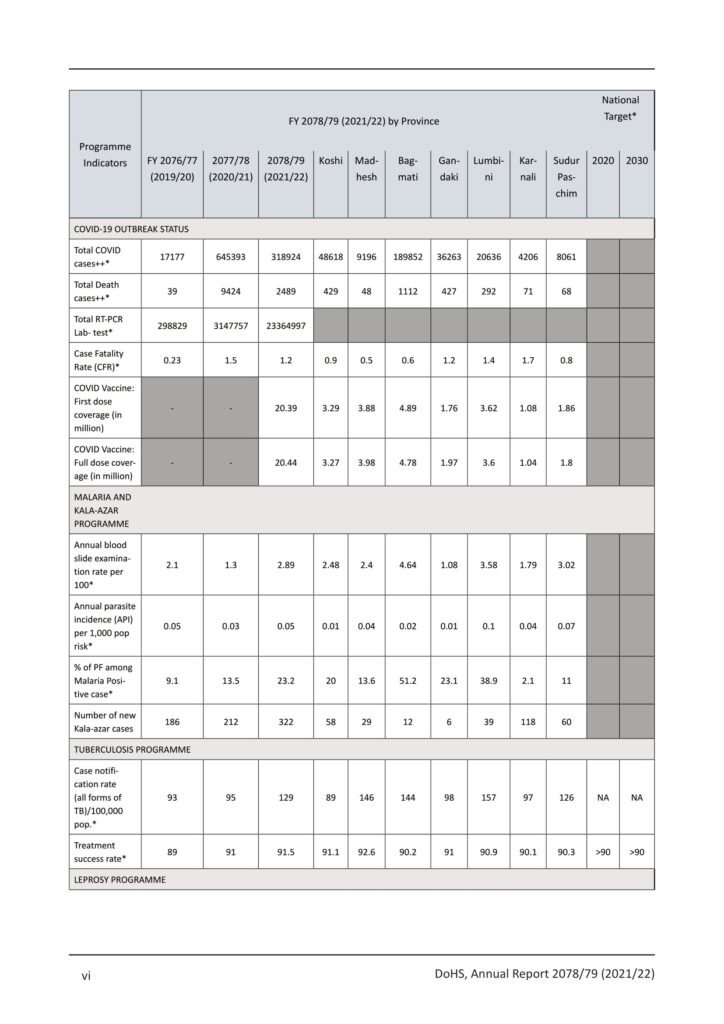
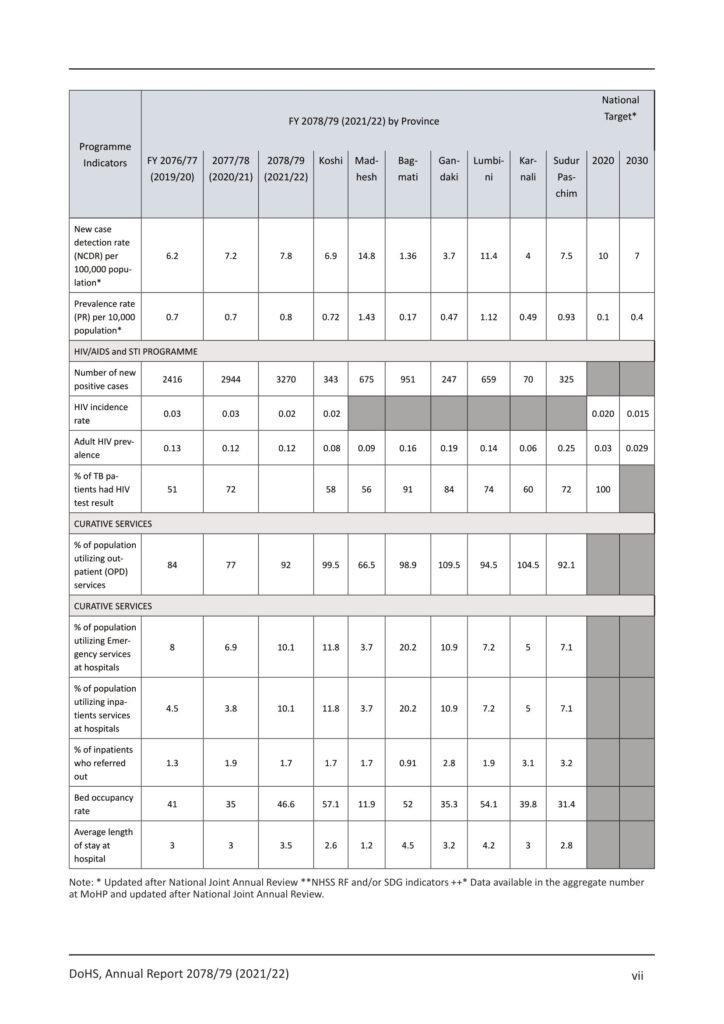
- Department Health Services (DoHS) Annual Report 2078/79 (2021/22)
- Nepal Health Sector Strategic Plan 2023-2030
- Annual Report of the Department of Health Services (DoHS) 2077/78
- Glimpse of Annual Report Department of Health Services 2073/74 (2016/17)
- Annual report of the Department of Health Services (DoHS) 2073/74 (2016/2017)
- Annual Report Department of Health Services 2072/73 (2015/2016)
- Annual Report of the Department of Health Services (DoHS) – 2071/72 (2014/2015)
- Annual Report of DOHS 2070/71 (2013/2014)
- Annual Report of DoHS 2069/2070 (2012-2013)
- National Annual Review, MoHP – 2017/18 (Presentation Slides)
- Health Sector Progress Report 2018, Ministry of Health & Population
- Glimpse of Annual Report Department of Health Services 2073/74 (2016/17)
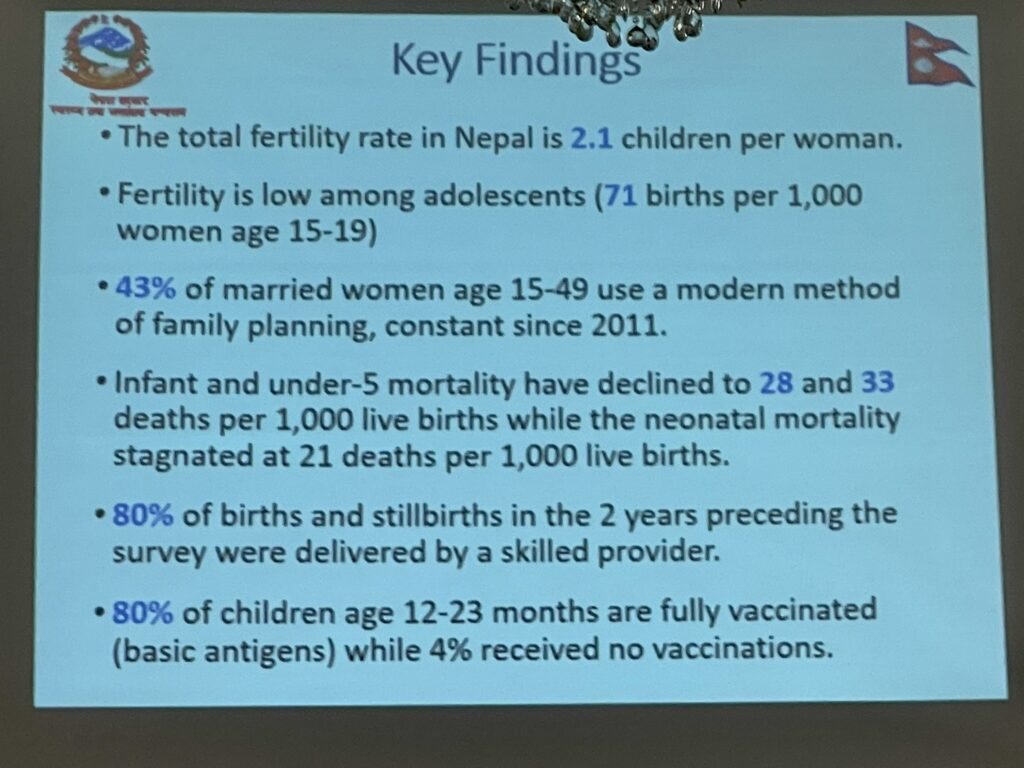
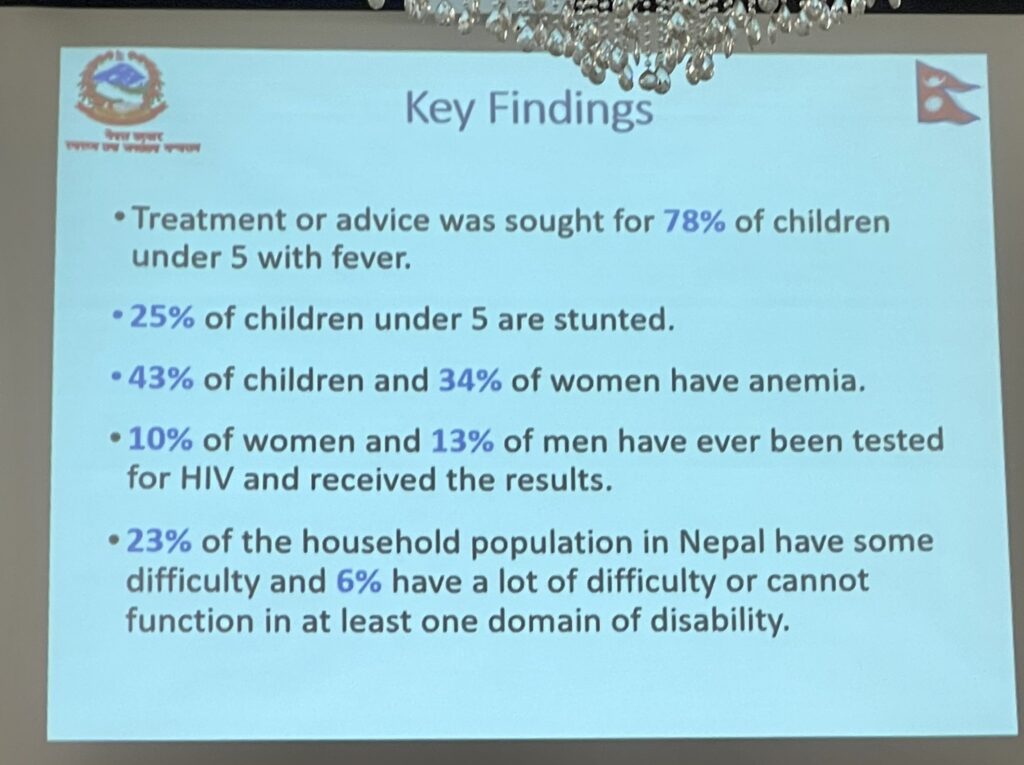
- Key Findings (Nepali & English) – The 2016 Nepal Demographic and Health Survey (2016 NDHS)
- Nepal Health Sector Strategy(NHSS) Implementation Plan 2016-21








![Vacancy Announcement for Nurses [Nepal-UK G2G Agreement] 49 1](https://publichealthupdate.com/wp-content/uploads/2023/07/1-736x1024.jpeg)
![Vacancy Announcement for Nurses [Nepal-UK G2G Agreement] 50 F1hXEQhaEAAkKf3](https://publichealthupdate.com/wp-content/uploads/2023/07/F1hXEQhaEAAkKf3-818x1024.jpeg)
![Vacancy Announcement for Nurses [Nepal-UK G2G Agreement] 51 appflowchart](https://publichealthupdate.com/wp-content/uploads/2023/07/appflowchart-1024x858.png)



![Nepal Demographic and Health Survey 2022 [Key Findings] Nepal Demographic and Health Survey 2022 [Key Findings]](https://publichealthupdate.com/wp-content/uploads/2023/06/NDHS-1170x830.png)
![Nepal Demographic and Health Survey 2022 [Key Findings] 71 655d7ee1 0a3a 470a 8d55 8b790f2d14f7](https://publichealthupdate.com/wp-content/uploads/2023/06/655d7ee1-0a3a-470a-8d55-8b790f2d14f7.png)
![Nepal Demographic and Health Survey 2022 [Key Findings] 72 GF56 1](https://publichealthupdate.com/wp-content/uploads/2023/06/GF56-1-1024x791.jpg)
![Nepal Demographic and Health Survey 2022 [Key Findings] 73 GF56 2](https://publichealthupdate.com/wp-content/uploads/2023/06/GF56-2-1024x791.jpg)









![Progress of Health and Population Sector 2021/22 (2078/79 BS) [National Joint Annual Review Report] Progress of Health and Population Sector 2021/22 (2078/79 BS) [National Joint Annual Review Report]](https://publichealthupdate.com/wp-content/uploads/2022/11/Public-Health-Calendar.png)