Overview
The Sustainable Development Goals include the target of reducing the global maternal mortality ratio (MMR) to less than 70 per 100,000 live births, with no country having an MMR that exceeds twice the global average. Nepal has committed to reduce
the MMR from 281 per 100,000 live births in 2006 to 116 by 2022, 99 by 2025, and 70 by 2030. This Nepal Maternal Mortality Study 2021 is the first ever joint undertaking of the Ministry of Health and Population (MoHP), the National Statistics Office (NSO), the Nepal Health Research Council, and health development partners for estimating the MMR and identifying the causes of maternal deaths – during pregnancy, delivery, and postpartum periods – in Nepal. By doing so, it intends to inform evidence-based policies and programs at the federal, provincial, and local levels.
Brief Methodology
The MoHP, in collaboration with the NSO, made an arrangement through a Memorandum of Understanding, where the census enumerators, as a part of their regular work, collected data on live births and deaths of women of reproductive age (WRA) in the enumerated households for the last 12 months preceding the National Population and Housing Census 2021. In the first phase, those Census enumerators then completed the death notification forms to identify pregnancy-related deaths, and submitted them to the census supervisor and notified the deaths to the pre-identified and trained local level health workers. In the second phase of the study, the local level health workers visited the household of each of the deceased women, verified the information and identified the pregnancy related deaths. For each pregnancy-related death identified, a verbal autopsy was conducted by trained health workers using the verbal autopsy form.
Major Findings
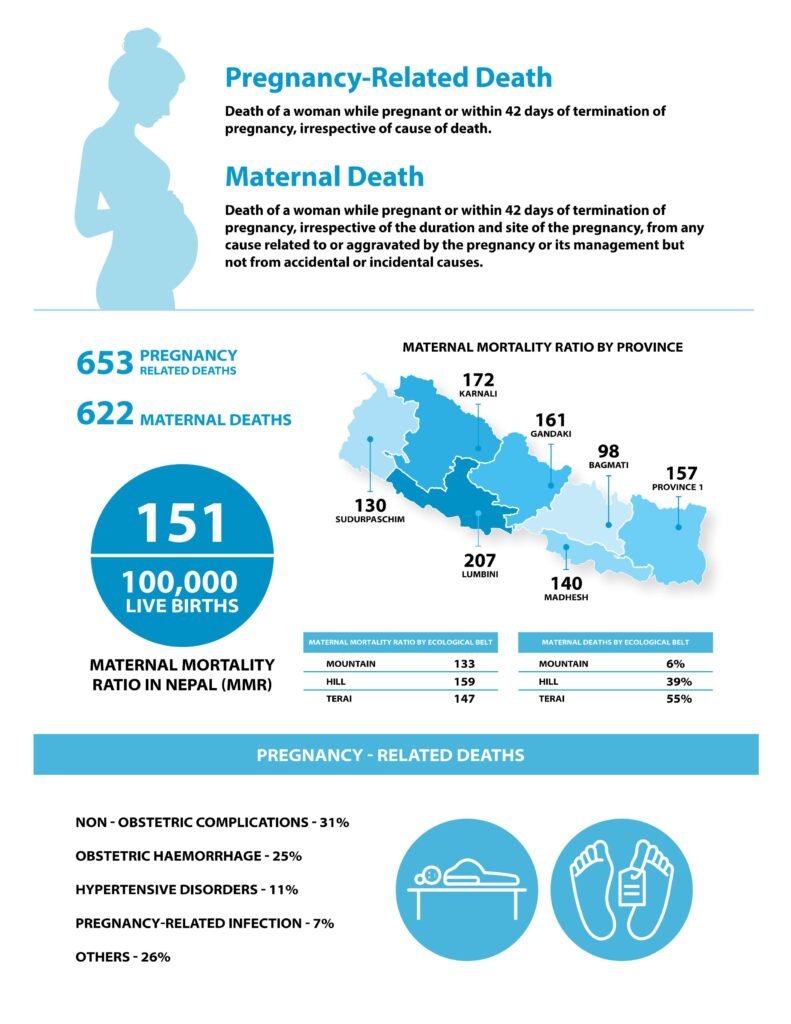
The MMR was found to be 151 per 100,000 live births in Nepal.
The MMR was found to be 151 per 100,000 live births in Nepal, with higher ratios in the Lumbini and Karnali provinces (207 and 172 per 100,000 live births respectively) and a lowest ratio in the Bagmati province (98 per 100,000 live births). Of the 12,976 deaths among women of reproductive age (15-49 years), 653 were pregnancy-related, comprising five percent of the total deaths in this age group.
- Of the 653 pregnancy-related deaths, 622 (95 percent) were classified as maternal deaths. The overall proportion of maternal deaths among the deaths of women of reproductive age was 4.8 percent. Only 611 maternal deaths were analysed further for causes and other attributes due to lack of sufficient information for 11 maternal deaths.
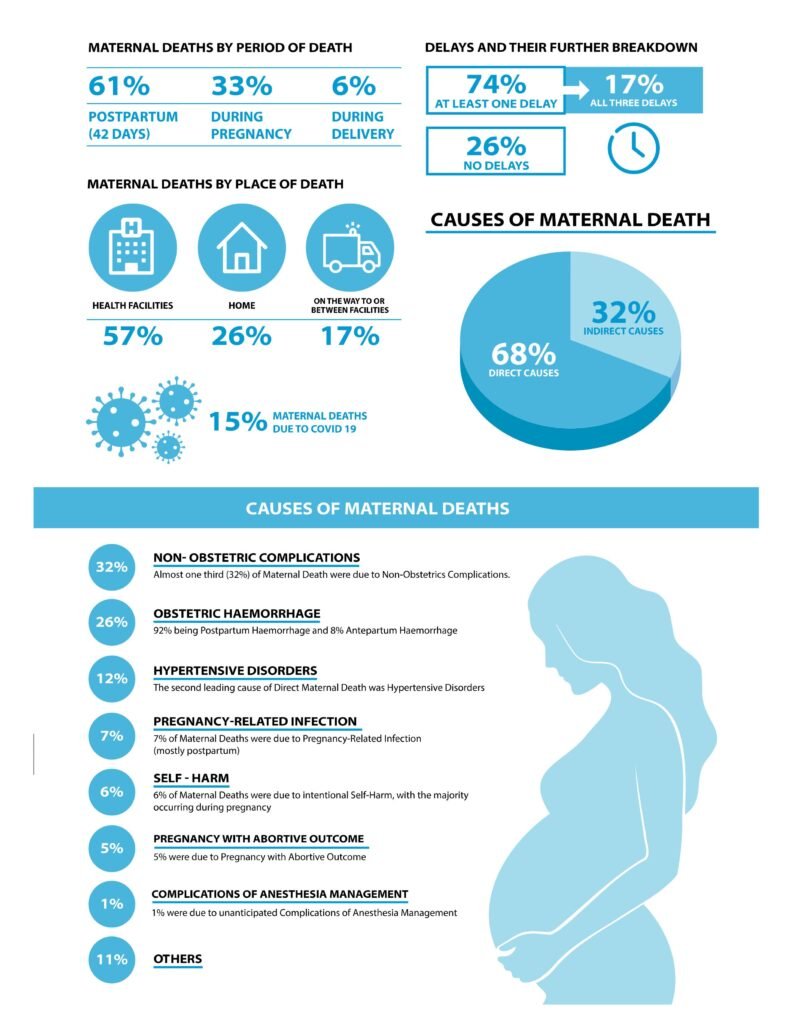
- The majority of the maternal deaths occurred in the postpartum period (61 percent), while thirty-three percent occurred during pregnancy and six percent during delivery. Nearly half of the deaths (47 percent) were reported in the Lumbini and Madhesh provinces. One in ten maternal deaths was among adolescent mothers. The majority of the deaths (57 percent) occurred in health facilities, whereas 26 percent occurred at home.
- Out of 412 women who died during delivery and postpartum period, fifty-three percent had attended all four antenatal care visits; while of the 173 women who died between 7-42 days of delivery 45 percent had attended all three postnatal care visits as per the protocol.
- Among the women who had died during delivery and in the postpartum period, over three-fourth (76 percent) had delivered at health facilities. Among those, 62 percent had delivered at government facilities while 38 percent at non- government health facility.
- Twenty-seven percent of women who died during the postpartum period had excessive bleeding, 23 percent had experienced dizziness and fainting, and 12 percent had been afflicted by fits and seizures. Eighty- three percent of the deceased had sought treatment for illness at a health facility or other place before death. Among those who did not seek treatment, nearly half did not consider it necessary (48%).
- The largest cause of maternal death was found to be non-obstetric complications (indirect maternal deaths) (32 percent). This was followed by obstetric haemorrhage (26 percent) and hypertensive disorders (12 percent). Five percent of the deaths were attributable to pregnancies with abortive outcomes. The leading causes of death during pregnancy were observed to be non-obstetric complications (40 percent), followed by direct deaths without obstetric codes (17 percent), and hypertensive disorders (14 percent). On the other hand, more than three quarters (78 percent) of deaths during delivery were attributable to obstetric haemorrhage. For deaths during the postpartum period, nearly a third were due to obstetric haemorrhage and non- obstetric complications (31 percent each).
- In connection to the “Three Delays” that lead to pregnancy-related mortality, a majority (74 percent) of the deceased women had experienced at least one type of delay, while 17 percent had experienced all three delays.
- The most common was the delay in seeking appropriate care (57 percent), followed by delay in receiving appropriate care (40 percent), and delay in reaching the healthcare facility for care (33 percent).
Conclusion
- In conclusion, the study showed that many maternal deaths in Nepal are due to preventable causes such as haemorrhage and high blood pressure during pregnancy, but a significant number are also caused by non- obstetric complications such as intentional self-harm. It highlighted the importance of improving the quality of maternal health services in health facilities and strengthening referral mechanisms, emergency transportation, and early screening for danger signs.
- In addition of its potential to strengthen community-based maternal death surveillance and response in the country, the NMMS 2021 also sets a precedent for conducting nationwide censuses of maternal deaths in future censuses to estimate the MMR and identify causes of death.
[Excerpt from Executive summary]
Download Report: National Population and Housing Census 2021: A Report on Maternal Mortality
Recommended readings
- Key Indicators: The Nepal Demographic and Health Survey (1996 NDHS- 2016 NDHS)
- The 2016 Nepal Demographic and Health Survey (2016 NDHS)
- Nepal Multiple Indicator Cluster Survey 2019 (NMICS 2019): Key findings
- Organogram and Reporting Mechanism of Nepalese Health System in Federal Context
- The 2015 Nepal Health Facility Survey: Further Analysis Reports
- Key findings – The 2015 Nepal Health Facility Survey (2015 NHFS)
- Nepal Health Facility Survey (2015 NHFS) Preliminary Report
- Health Facility Operation and Management Committee- A reference guideline for local level
- Nepal Health Facility Registry, MoHP
- Health Facility Operation Standards, 2077
- Health Facility Quality Improvement Module (QI Tool) for Health Services Strengthening


