Among them 15,655 (46%) were new smear
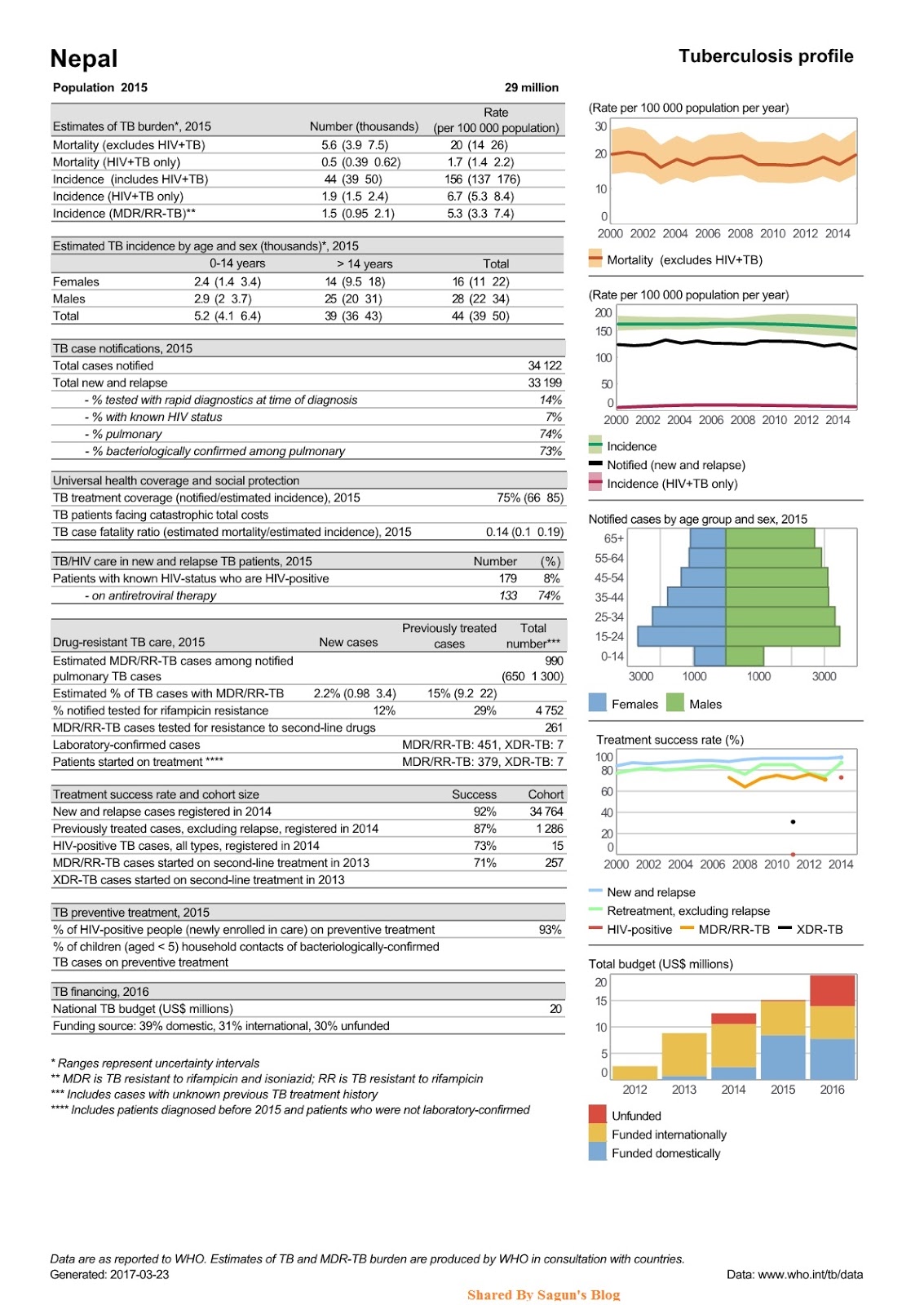
positive TB cases, 2,202 (6%) were smear positive retreatment cases, 6,686 (20%) were sputum smear negative and 8,966 (26%) were extra‐pulmonary TB cases. Out of total registered cases in NTP, there were 12,300 (36%) female and 21,821 (64%) male. According to the latest WHO data published in May 2014, tuberculosis deaths in Nepal reached 5,506. This is 3.5% of total deaths. The age adjusted death rate is 27.80 per 100,000 of population. This ranks Nepal as 43 in the world.A total of 4244 DOTS treatment centers are providing TB treatment service. Expansion of this cost effective and highly successful treatment strategy has proven its efficacy in reducing the mortality and morbidity in Nepal. The NTP has coordinated with the public sectors, private sectors, local government bodies, I/NGOs, social workers, educational sectors and other sectors of society in order to sustain the present significant results achieved by National Tuberculosis Program (NTP).
- To dramatically reduce the National burden of TB by 2015 in line with the Millennium Development Goals and the Stop TB Partnership targets
- Achieve universal access to high‐quality diagnosis and patient‐centered treatment
- Reduce the human suffering and socioeconomic burden associated with TB
- Protect poor and vulnerable populations from TB, TB/HIV and multi‐drug‐resistant TB
- MDG 6, Target 8: …halted by 2015 and begun to reverse the incidence.
- Targets linked to the MDGs and endorsed by the Stop TB Partnership:
- By 2005: detect 100% of new sputum smear‐positive TB cases and cure at least 85%of these cases.
- By 2015: reduce prevalence of and death due to TB by 50% relative to 1990.
- By 2050: eliminate TB as a public health problem (<1 case per million population).
- Political commitment with increased and sustained financing
- Case detection through quality‐assured bacteriology
- Standardized treatment with supervision and patient support
- An effective drug supply and management system
- Monitoring and evaluation system, and impact measurement
2. Address TB/HIV, DR‐TB and other challenges
- Implement collaborative TB/HIV activities
- Prevent and control multi‐drug‐resistant TB
- Address prisoners, refugees and other high‐risk groups and special situations
- Actively participate in efforts to improve system‐wide policy, human resources, financing,management, service delivery, and information systems
- Share innovations that strengthen systems, including the Practical Approach to Lung Health (PAL)
- Adapt innovations from other fields
- Public‐Public, and Public‐Private Mix (PPM) approaches
- International Standards for Tuberculosis Care (ISTC)
5. Empower people with TB, and communities
- Advocacy, communication and social mobilization
- Community participation in TB care
- Patients’ Charter for Tuberculosis Care
- Programme‐based operational research