National Guideline on Prevention, Management and Control of Dengue in Nepal
Overview
Dengue infection is a systemic and dynamic disease and has a wide clinical spectrum that includes both severe and non severe clinical manifestations. For a disease that is complex in its manifestations, management is relatively simple, inexpensive and very effective in saving lives so long as correct and timely interventions are instituted. The key is early recognition and understanding of the clinical problems during the different phases of the disease, leading to a rational approach to case management and a good clinical outcome.
Early notification of dengue cases seen in primary and secondary care is crucial for identifying outbreaks and initiating an early response.
Step wise approach for case management
Step 1: Overall Assessment
Step 2: Diagnosis, Assessment of Disease Phase and Severity
Step 3: Clinical Management
1.1 History, including symptoms, past medical and family history
1.2 Physical examination, including full physical and mental assessment
1.3 Investigation, including routine laboratory tests and dengue-specific laboratory tests
2 Clinicians will diagnose whether the disease is dengue and assess its phase and severity
3.1 Disease notification
3.2 Management decisions
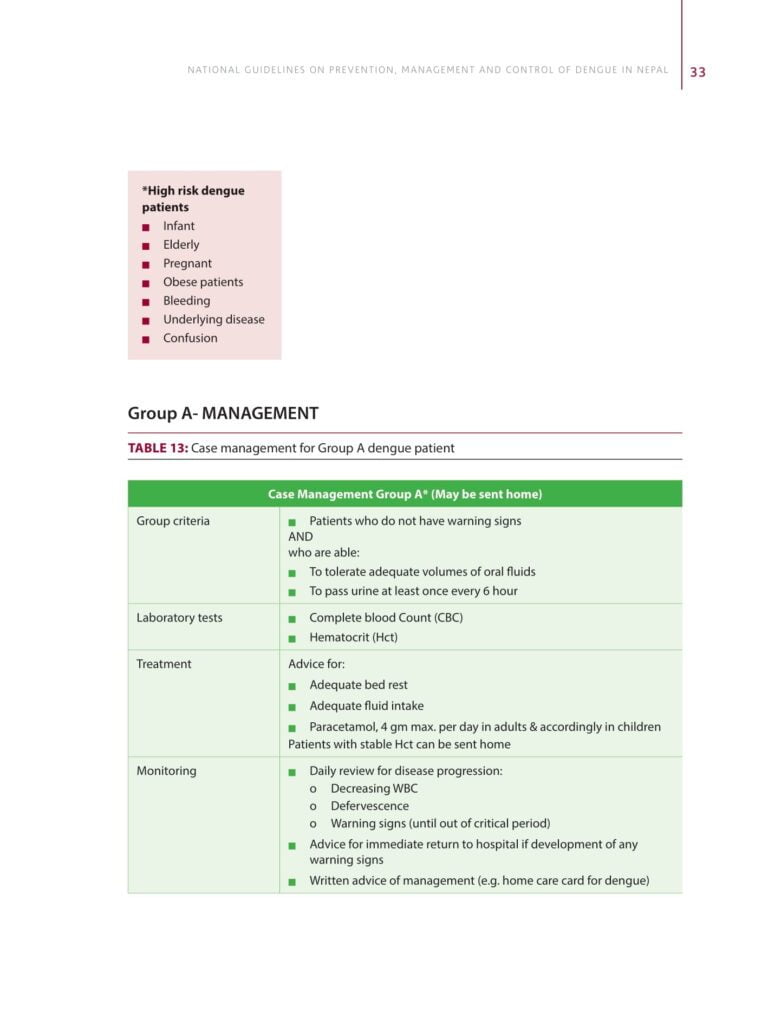
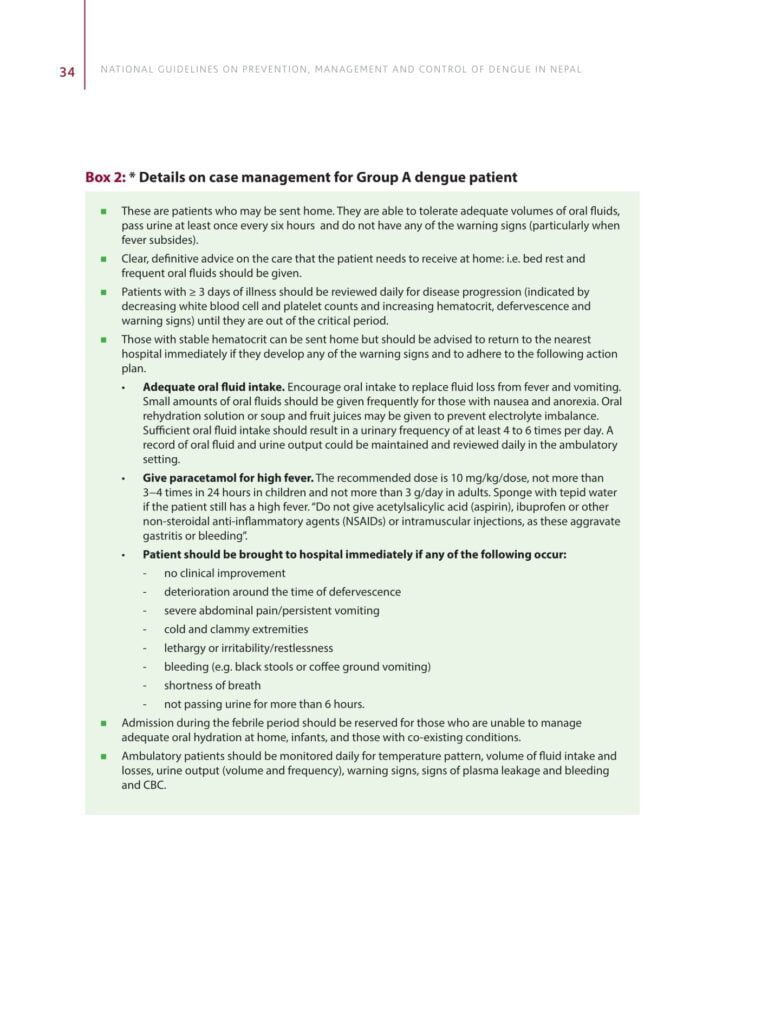
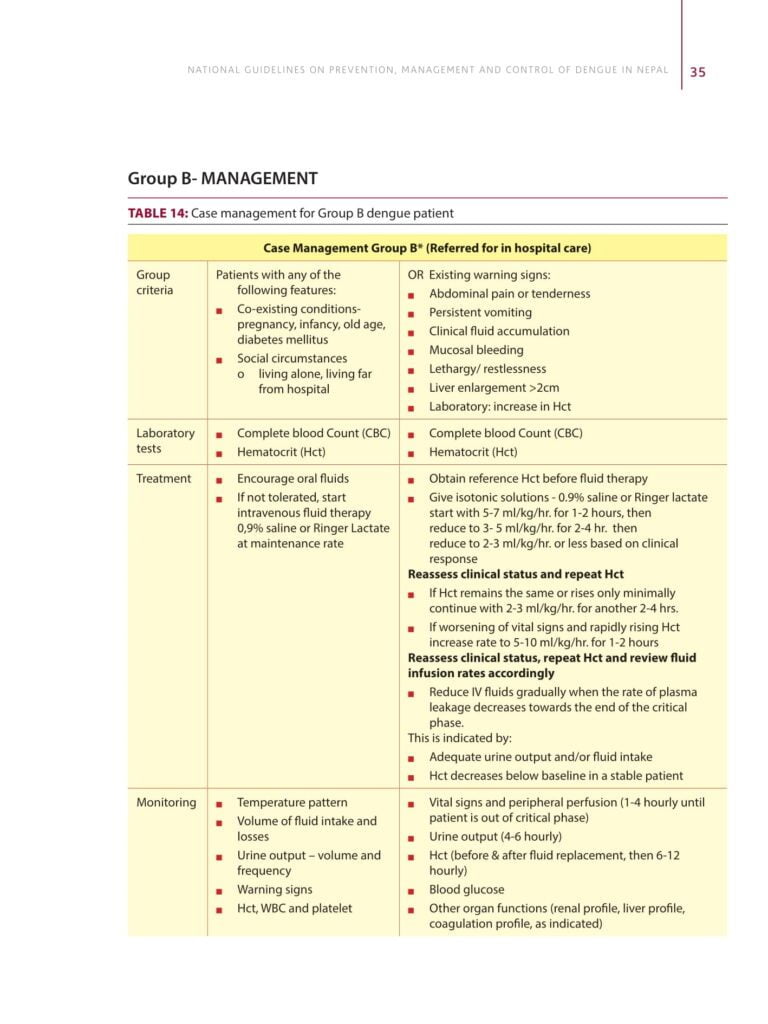
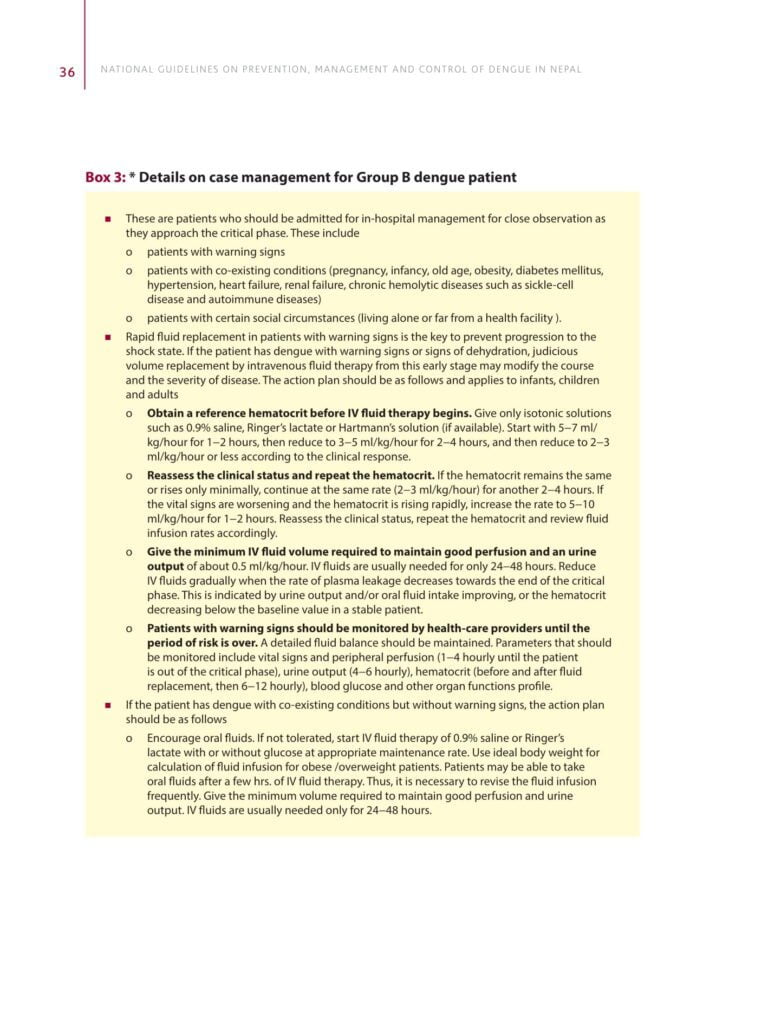
Depending on the clinical manifestations and other circumstances, patients may
– be sent home (Group A)
– be referred for hospital management (Group B)
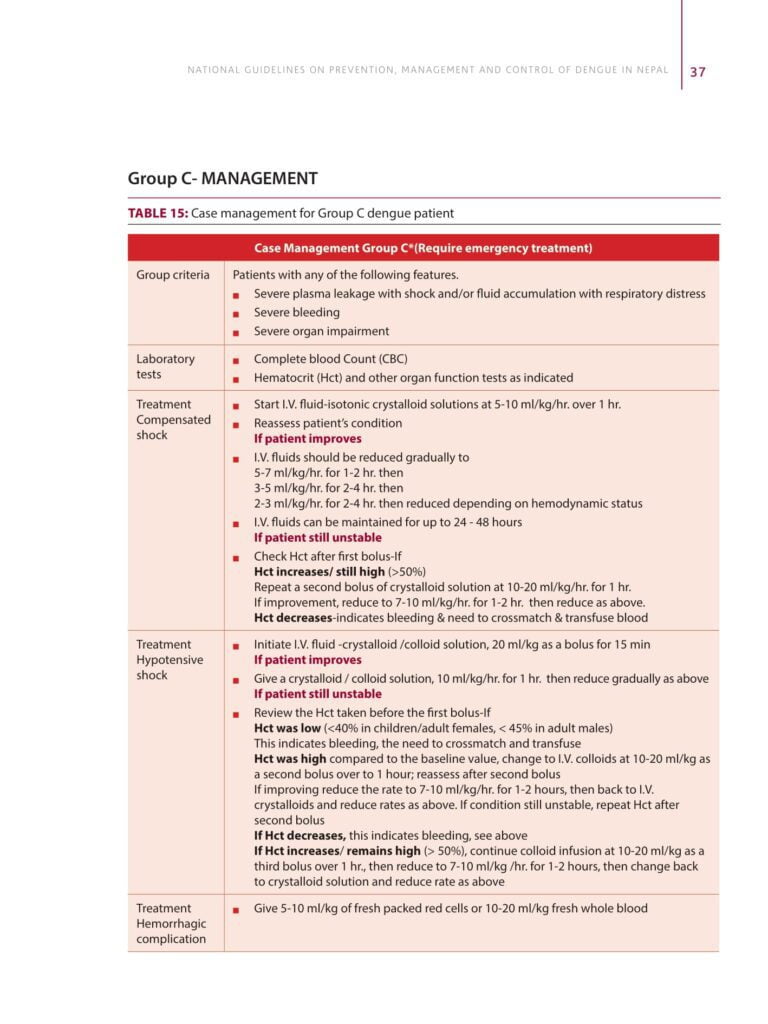
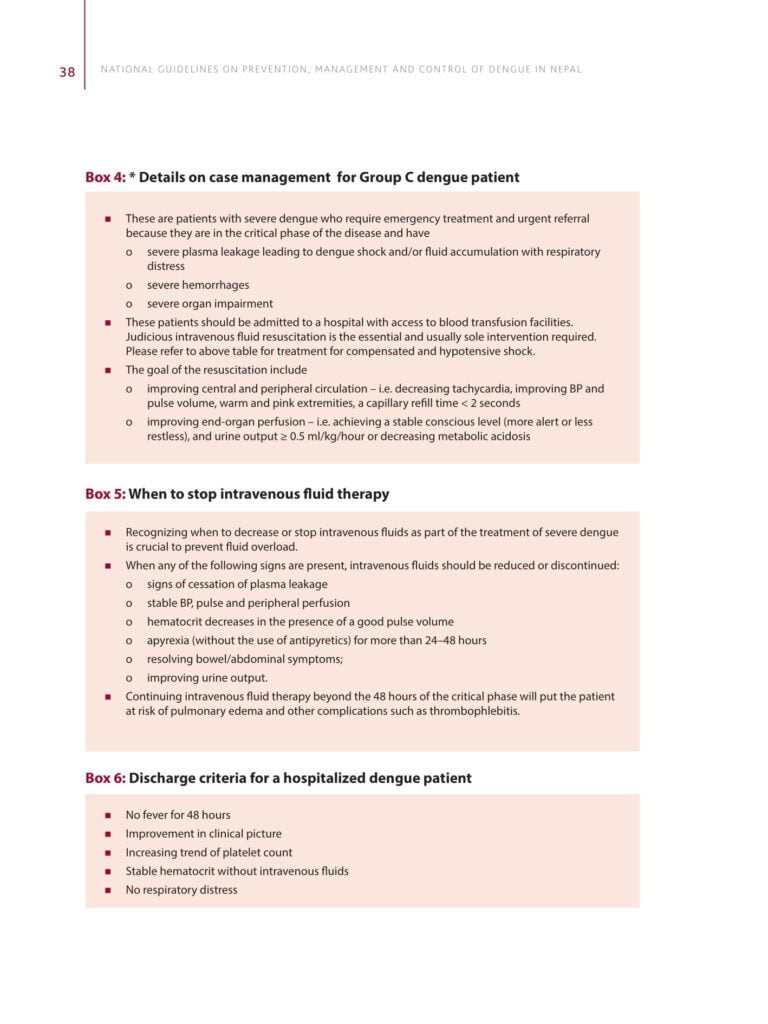
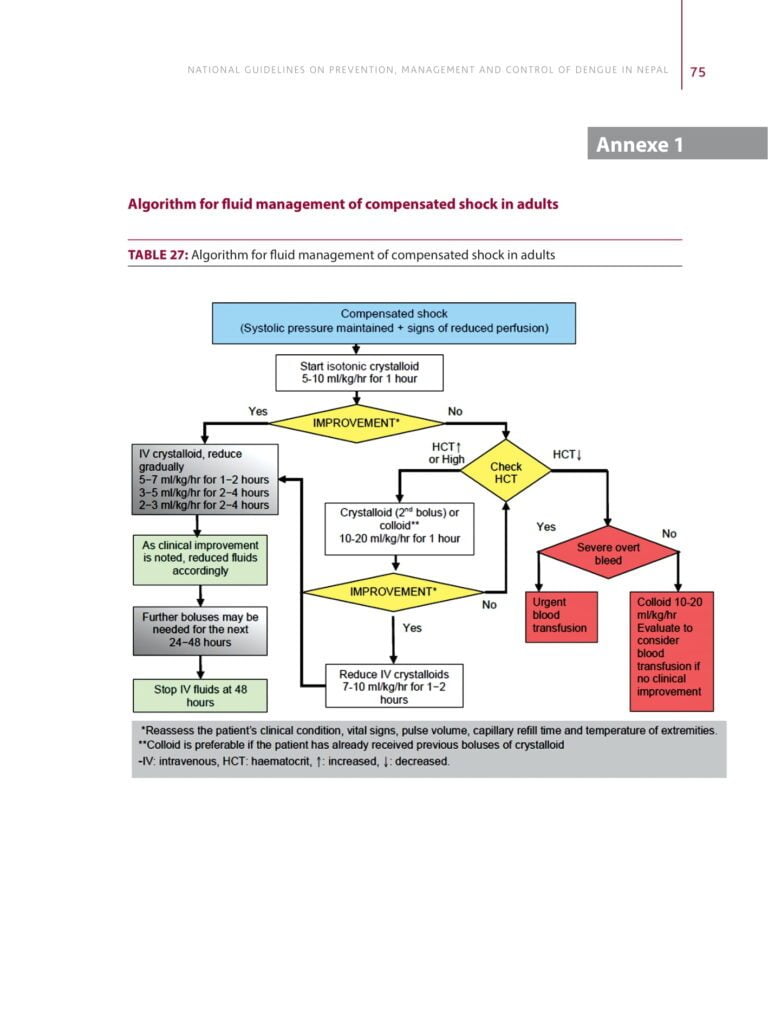
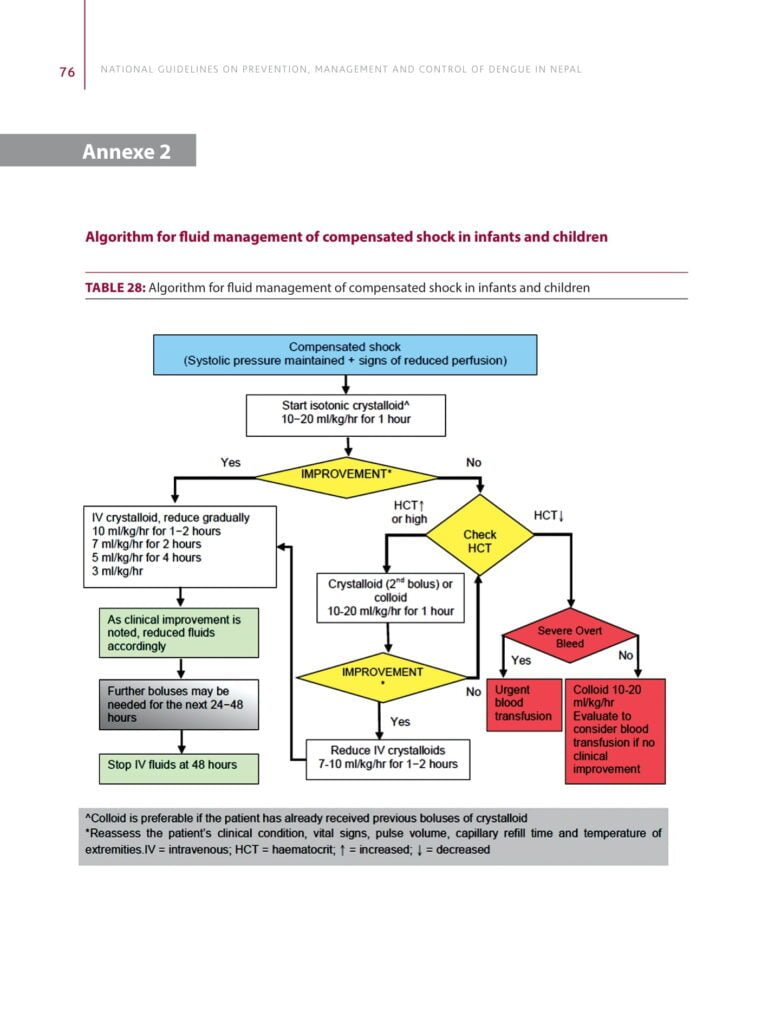
– require emergency treatment and urgent referral (Group C)
Step 1 Overall Assessment
History
– date of onset of fever/illness
– quantity of oral fluid intake
– diarrhea
– urine output (frequency, volume and time of last voiding)
– assessment of warning signs
– change in mental state/seizure/dizziness
– other important relevant history, such as family or neighborhood dengue, travel to dengueendemic areas, co-existing medical conditions.
Physical examination
– assessment of mental state
– assessment of hydration status
– assessment of hemodynamic status
– checking for quiet tachypnoea/acidotic breathing/pleural effusion
– checking for abdominal tenderness/hepatomegaly/ascites
– examination for rash and bleeding manifestations
– tourniquet test (repeat if previously negative or if there is no bleeding manifestation)
Investigation
Details on investigation is provided in chapter 3
– CBC: A complete blood count should be done at the first visit (it may be normal), CBC should be repeated daily until the critical phase is over. Decreasing white blood cell and platelet counts make the diagnosis of dengue very likely.
– Hematocrit: The hematocrit in the early febrile phase could be used as the patient’s own baseline.
Note
– Leukopenia usually precedes the onset of the critical phase and has been associated with severe disease.
– A rapid decrease in platelet count, concomitant with a rising hematocrit compared to the baseline, is suggestive of progress to the plasma leakage/critical phase of the disease. These changes are usually preceded by leukopenia (≤ 4000 cells/mm3).
– In the absence of the patient’s baseline, age-specific population hematocrit levels could be used as a surrogate during the critical phase.
– Dengue-specific laboratory tests can be performed to confirm the diagnosis. However, it is not necessary for the acute management of patients, except in cases with unusual manifestations.
– Additional tests should be considered in patients with co-morbidities and severe disease as indicated.
These may include tests of liver function, glucose, serum electrolytes, urea and creatinine, bicarbonate or lactate, cardiac enzymes, electrocardiogram (ECG) and urine specific gravity.
Step 2
Diagnosis, assessment of disease phase and severity
On the basis of evaluations of the overall assessment as described above, clinicians should determine whether the disease is dengue, which phase it is in (febrile, critical or recovery), whether there are warning signs, the hydration and hemodynamic state of the patient, and whether the patient requires admission or not.
Step 3
Disease notification and management decision
Disease notification
In dengue-endemic countries like Nepal, cases of suspected, probable/highly suggestive and confirmed dengue should be notified early so that appropriate public-health measures can be initiated. Laboratory confirmation is not necessary before notification, but if available should be reported. Notification of dengue is mandatory in Nepal. It is also a part of early warning and reporting system (EWARS) and should be reported accordingly.
Management decisions
Depending on the clinical manifestations and other circumstances, patients may either
– be sent home (Group A)
– be referred for in-hospital management (Group B) or
– require emergency treatment and urgent referral (Group C)

Please refer Step wise approach for National Guideline on Prevention, Management and Control of Dengue in Nepal


