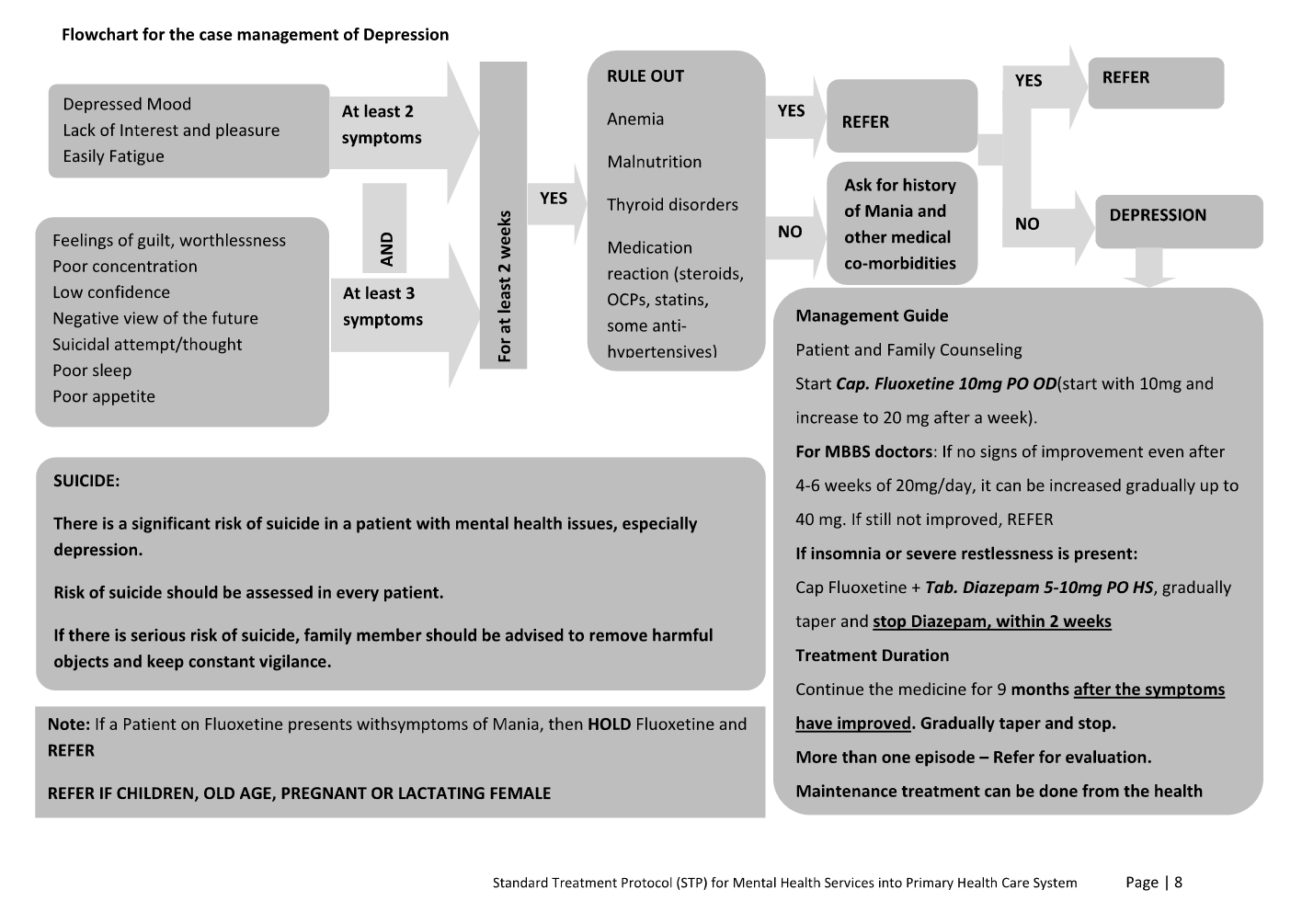
- When insomnia or severe restlessness is present: Add Tab. Diazepam 5mg PO HS along with fluoxetine. Decrease the dose to 2.5mg after 1 week and then stop Diazepam within 2 weeks. Do not give diazepam for more than 2 weeks.
- Stop the medication and refer whenever there are symptoms of mania.
Depression: let’s talk – 7 April 2017 | World Health Day
Depression: let’s talk – 7 April 2017 | World Health Day
Depression: let’s talk – 7 April 2017 | World Health Day